Tumor
cells gain access to the leptomeninges by hematogenous dissemination or by direct
extension. Once these cells reach the CSF, they are disseminated throughout the neuraxis
by the constant flow of CSF. The CSF travels from the ventricles through the foramen of
Magendie and Luschka to the spinal canal and over the cortical convexities to the
arachnoid granulations. Infiltration of the leptomeninges by any malignancy is a serious
complication that results in substantial morbidity and mortality.
Neoplastic meningitis occurs in approximately 5% of
patients with cancer. This disorder is being diagnosed with increasing frequency as
patients live longer and as neuroimaging studies improve. The most common cancers to
involve the leptomeninges are breast cancer, lung cancer, and melanoma. Without
treatment, the median survival of patients diagnosed with this disorder is 4 to 6 weeks,
with death resulting from progressive neurologic dysfunction.
The goals of treatment in patients with leptomeningeal
metastases are to improve or stabilize the neurologic status of the patient and to prolong
survival. Standard therapy involves RT to
symptomatic sites of the neuraxis and to disease visible on neuroimaging studies, in
addition to intrathecal chemotherapy. These therapies increase the median survival to 3 to
6 months and often provide effective local control, allowing patients to die from
systemic rather than neurologic complications of their neoplasm. Early diagnosis and
therapy are critical to preserving neurologic function.
Patient Evaluation
Patients present with signs and symptoms ranging from
injury to nerves that traverse the subarachnoid space, direct tumor invasion of the brain
or spinal cord, alteration in the local blood supply, obstruction of normal CSF flow
pathways leading to increased intracranial pressure, or interference with normal brain
function. Patients should have a physical examination with a careful neurologic
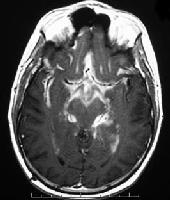
evaluation; MRI of the brain and spine should also be done, if the patient has appropriate
neurologic symptoms or signs. A definitive diagnosis is most commonly made by lumbar
puncture. The CSF protein is typically increased, and there may be a pleocytosis or
decreased glucose levels. The CSF cytology is positive approximately 50% of the time
with the first lumbar puncture, and 85% of the time after three CSF examinations in
patients who are ultimately proven to have neoplastic meningitis. However, the CSF
cytology is persistently negative in 10% to 15% of patients with leptomeningeal
carcinomatosis. In these cases, (1) a suspicious CSF examination (eg, increased protein,
low glucose, and/or a pleocytosis) combined with suggestive clinical findings (eg,
multifocal neuraxis involvement, such as cranial nerve palsies and a lumbar radiculopathy
that cannot be explained otherwise); and/or (2) suggestive radiologic features (eg,
subarachnoid masses, diffuse contrast enhancement of the meninges, or hydrocephalus
without a mass lesion) can be sufficient to treat when the patient is known to have a
systemic malignancy. Although a positive CSF cytology in patients with solid tumors is
virtually always diagnostic, reactive lymphocytes from infections (eg, herpes zoster
infection) can often be mistaken for malignant lymphocytes.
Patient Stratification for Treatment
Once the diagnosis has been
established, the patient's overall status should be carefully assessed to determine how
aggressively the carcinomatous or lymphomatous meningitis should be treated.
Unfortunately, this disease is most common in patients with advanced, treatment-refractory
systemic malignancies for whom treatment options are limited. In general, fixed neurologic
deficits (such as cranial nerve palsies or paraplegia) do not resolve with therapy,
although encephalopathies may improve dramatically. As a result, patients should be
stratified into “poor risk” and “good risk” groups.
The poor-risk group includes patients with a low KPS; multiple, serious, fixed neurologic
deficits; extensive systemic disease with few treatment options; bulky CNS disease; and
neoplastic meningitis related to encephalopathy. The good-risk group includes patients
with a high KPS, no fixed neurologic deficits, minimal systemic disease, and reasonable
systemic treatment options. Many patients fall in between these two groups, and clinical
judgment will dictate how aggressive their treatment should be.
Treatment Algorithm for Neoplastic Meningitis
Patients in the poor-risk group are usually offered
supportive care measures. RT is commonly administered to symptomatic sites (eg, to the
whole brain for increased intracranial pressure or to the lumbosacral spine for a
developing cauda equina syndrome). If the patient stabilizes or improves, a more
aggressive treatment approach may be considered. Patients with exceptionally
chemosensitive tumors (eg, small cell lung cancer, lymphoma) may be treated.
Good-risk patients can receive radiation to symptomatic
sites and to areas of bulky disease identified on neuroimaging studies. In addition,
intrathecal or intraventricular (using a surgically implanted subcutaneous reservoir and
ventricular catheter [SRVC]) chemotherapy can be administered; systemic chemotherapy can
be considered. Initially, intrathecal chemotherapy is usually given by lumbar puncture,
and the SRVC is placed later to administer the drugs more conveniently. Initiation of
chemotherapy should not be delayed for flow study. When dosing intrathecal chemotherapy
for adults, no adjustment is made based on weight or body surface area. With methotrexate,
thiotepa, and cytarabine, a typical dosing schedule is initially twice a week for 4 weeks;
if the CSF cytology becomes negative, then continue with once-a-week administration of
intrathecal chemotherapy for another 4 weeks, followed by once-a-month maintenance doses.
Methotrexate (10-12 mg) is the drug most frequently used for intrathecal administration.
Oral leucovorin (folinic acid) can be given (10 mg twice a day for 3 days starting the day
of treatment) to reduce possible systemic toxicity without interfering with the efficacy
of methotrexate in the CSF. Intrathecal thiotepa (10 mg) can also be used in solid tumors,
and cytarabine (50 mg) is often administered for lymphomatous meningitis. A depot form of
cytarabine is now available that allows patients with lymphomatous meningitis to be
treated every 2 weeks initially (rather than twice per week) followed by once-a-month
maintenance treatment. In a randomized controlled trial, depot cytarabine was found to
increase the time to neurologic progression, with a response rate comparable to
methotrexate, while offering the benefit of a less demanding schedule of injection. One
study suggests that high-dose systemic methotrexate might be better than intrathecal
therapy. If an SRVC is placed, a CSF flow scan should be strongly considered. CSF flow
abnormalities are common in patients with neoplastic
meningitis and often lead to increased intracranial pressure. Administering chemotherapy
into the ventricle of a patient with a ventricular outlet obstruction increases the
patient's risk for leukoencephalopathy. In addition, the agent administered will not reach
the lumbar subarachnoid space where the original CSF cytology was positive. CSF flow scans
are easily performed in most nuclear medicine departments. Indium 111-DTPA is administered
into the SRVC, and imaging of the brain and spine is performed immediately after injection
and then imaging is done again at 4 and 24 hours. If significant flow abnormalities are
seen, RT is administered to the sites of obstruction and a CSF flow scan is repeated. If
CSF flow normalizes, which occurs most commonly in radiosensitive neoplasms, intrathecal
chemotherapy commences. If significant flow abnormalities remain, then the patient should
be treated as a poor-risk patient (ie, with supportive measures). For patients with a
normal CSF flow scan and otherwise stable disease, induction intrathecal chemotherapy
should be given for 4 to 6 weeks (see ) and then the patient should be reassessed
clinically and with a repeat CSF cytology. Because the cytology is much less likely to be
positive from the SRVC than from the lumbar subarachnoid space, it is critical that it be
sampled from the site where the cytology was originally positive. If the CSF cytology was
originally negative, then reassess from the lumbar region. If the patient is clinically
stable or improving and there is no clinical or radiologic evidence of progressive
leptomeningeal disease, the patient should receive another month of “induction”
intrathecal chemotherapy or should consider switching intrathecal drugs for 4 weeks. This
regimen should be followed by 1 week per month of maintenance therapy if the cytology has
converted to negative. The CSF cytology status should be followed every month.
Progressive Disease
The patient's clinical and CSF
status should be followed every 2 months. However, if the patient's clinical status is
deteriorating from progressive leptomeningeal disease or if the cytology is persistently
positive, the clinician has two options: (1) chemotherapy; (2) supportive care, which may
include RT to symptom sites. |